THE MEDICALIZATION OF OLD
AGE
Like religion and law, medicine is a moral enterprise as it defines
and manages individuals deemed undesirable by the broader culture (Eliot
Freidson, The Profession of Medicine). Over the course of the twentieth
century, deviance has increasingly been medicalized, as is evident in our
public discourse: one is no longer a drunkard but rather "suffers"
from alcoholism; the slow-learner in school is no longer stupid but rather
has a "learning disorder;" and instead of viewing the disorientations
of older persons being the result of personal and social change, they are
viewed as symptoms of "senility."
If it is the contemporary old who are trailblazing a new stage of
the life-cycle, then it is the physician
who is their trail guide. In mass media advice columns, public seminars
and professional journals, it is the physician who informs the elderly
on such non-biological matters as retirement, friendships, finances and
leisure.
In the Greek tale of Tithonus, a beautiful young man asked Aurora, the
goddess of morning, to make him immortal. She does, and he ages continuously.
Finally, pitying his never-ending dissolution, she makes him into a grasshopper.
Consider medicine's role in the lives of those most likely to die in our
culture. Instead of making the oldest of the old into grasshoppers, the
medical establishment has produced a population requiring ever greater
services with advanced age--including the million or more nursing home
residents so disabled that twenty-four hour care is required, and the ten
thousand individuals existing in irreversible vegetative states. Old age
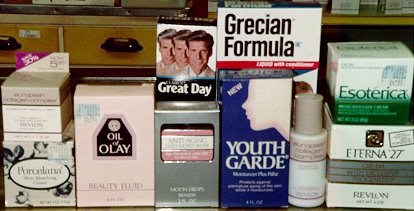
has increasingly become equated with the dying process. Our cultural gerontophobia
derives from our cultural thanatophobia; the myriad of anti-aging products
and services are in our youth-oriented culture, in actuality, potions and
rituals to avoid death. Click here for consequences
of medicine controlling the final rite-of-passage.
Medicine's Biases Against the Old
Given the medicalization of old age, the dramatic increases in their
numbers, and the fact that those 65 and older account for 44% of all days
spent in the hospital and one-third of the nation's health care expenditures,
it is ironic how, as of 1993, only eight of the nation's 126 medical schools
required separate courses in geriatric medicine and there were only about
4,000 board-certified geriatricians in the United States. Reasons for such
shortages vary: in the hierarchy of medical specialties (and its specialty
status is not fully recognized in the U.S., as it is in many north European
countries), geriatric medicine may not be the most glamorous nor lucrative;
care for older persons is not the most reinforcing professionally, with
irreversible physical declines and death being the long-term outcomes;
difficult (check out the paperwork required for Medicare and Medicaid)
and poor reimbursements for medical services; absence of professional role
models; and the negative aged stereotypes and death fears of physicians.
Whatever they are, the consequences have been significant. Among the stories
of medical mistreatment of older persons over the past decade are:
- a 1988 study by Rand Corporation researchers (Robert W. DuBois,
principle investigator) of the medical records of elderly patients who
died from three common illnesses at 12 hospitals found improper medical
care had caused the deaths of perhaps 27% of the cases;
- older persons are either over- or under-prescribed with medications,
and comprise more than one-half of all deaths from drug reactions (see "When Medicine Hurts Instead of Helps",
a report by the Alliance for Aging Research);
- people over 75 are less likely to receive prescriptions that reduce
heart-attacks, receiving clotbusting drugs one-sixth as often as younger
patients;
- while women over 65 are twice as likely to develop breast cancer
as younger women, those with the disease are one-half as likely to be treated
appropriately for it even though they are just as likely to benefit from
treatment;
- many elderly diabetics do not get recommended tests for their condition
in their doctor visits;
- between 25 and 40 percent of all acute hospital procedures performed
on older patients were found to be unnecessary
In addition, there are the home horror stories emerging from some of the nation's
16,700 nursing homes. For instance, in 1999, experts of the Nutrition Screening Initiative, a
broad coalition of health care groups, claimed that as many as 2 out of 5 of the nation's two
million nursing home residents are malnourished.
Nursing Homes and the Challenge of Long-term Care
 In our death-denying culture where one dies a series of mini deaths before
physiologically
expiring, where the dying process can be stigmatizing for both the dying and survivors-to-be,
the nursing home industry has emerged as depersonalization machines to absorb the shock of
the dying process. As Richard
Garvin and Robert E. Burger wrote in Where They Go to Die: The Tragedy of America's
Aged (1968), nursing homes are the "halfway houses between society and the
cemetery." In 1996, about $80 billion was spent on the care of 1.6 million Americans--
two-thirds of whom are women--residing in more than 17,000 nursing homes.
Three years earlier, in 1993, it was estimated that the use of nursing homes
would grow by 76% over the next 30 years.
In our death-denying culture where one dies a series of mini deaths before
physiologically
expiring, where the dying process can be stigmatizing for both the dying and survivors-to-be,
the nursing home industry has emerged as depersonalization machines to absorb the shock of
the dying process. As Richard
Garvin and Robert E. Burger wrote in Where They Go to Die: The Tragedy of America's
Aged (1968), nursing homes are the "halfway houses between society and the
cemetery." In 1996, about $80 billion was spent on the care of 1.6 million Americans--
two-thirds of whom are women--residing in more than 17,000 nursing homes.
Three years earlier, in 1993, it was estimated that the use of nursing homes
would grow by 76% over the next 30 years.
In the United States, nearly one-half of women and one-third of men will spend some
part of their lives in these
facilities before they die--25% for at least one year and 9% for five years or more, according to
the Health Care Financing Administration
(check out its "Guide to
Choosing a Nursing Home"). In 2002, Medicare put online a nursing home comparison
guide and a checklist
for rating different facilities. In 2006 appeared Consumer Report's
Nursing Home Guide.
Among the stories of nursing
home abuses over the past decade are:
- In 1988, according to a survey published by the Department of Health and Human
Services, more than one-quarter of the nation's nursing homes administered drugs without
regard to a physician's written orders.
- In a 1989 survey of 1,200 rest-home (otherwise labeled group homes or
domiciliary care facilities) residents in Massachusetts, whose care is not government-regulated,
more than half of the residents received mind-altering drugs, most without competent medical
supervision. In a 1991 study by University of Minnesota researchers of medical records from
60 nursing homes in 8 Western states from 1976-1985, about one in five residents had received
powerful tranquilizers but in only half of these cases were there written diagnoses justifying
their use.

- in 1990, before new Health Care Financing Administration regulations went into
effect, some 40% of nursing home residents were being either physically or chemically
restrained. That year it was reported that more than one-third of the nation's nursing homes
offering skilled care failed to meet standards for clean food in surprise inspections in 1988 and
1989, and nearly a quarter did not administer drugs properly.
- in 1997, the Florida-based Coalition to Protect the Nation's Elders called for
Congressional hearings on nursing home fraud and abuse. In it's 30-second television
commercial, it argues that some residents have been starved, beaten or left to die while
"giant
nursing home chains are ripping off taxpayers with phony billing scams."
- According to investigations of the General Accounting Office between 1995
and 1998, nearly one-third of California nursing homes were cited for violations that caused death or life-threatening harm to patients.
Following up on Time
magazine's 1997 investigative report, the GAO
found only 30 of the state's 1,370 nursing homes had passed state inspections
minimal or no problems
In 1996, the Clinton Administration considered scaling back inspections of many
nursing homes that care for elderly people under Medicaid and Medicare even though
government data showed more than two-thirds did not fully comply with federal standards
(which is required for Medicare and Medicaid reimbursements). The proposal was eventually dropped.
GERIATRIC MEDICINE RESOURCES
 According
to a report ("Geriatric
Medicine Training and Practice in the U.S. at the Beginning of the 21st Century")
of the American Geriatrics Society, in 1999, though comprising roughly 13% of
the total population, Americans 65 and older made 25% of the office visits to
physicians and were more than twice as likely as the overall population to be
hospitalized. And yet of the 144 medical schools in the country, there are
only 6 departments of geriatric medicine. Of the nearly 10,000 physicians
who graduated from family practice and internal medicine residency programs,
slightly more than 3% subsequently entered geriatric medicine fellowships. In
2001, there were only 9,000 certified geriatricians.
According
to a report ("Geriatric
Medicine Training and Practice in the U.S. at the Beginning of the 21st Century")
of the American Geriatrics Society, in 1999, though comprising roughly 13% of
the total population, Americans 65 and older made 25% of the office visits to
physicians and were more than twice as likely as the overall population to be
hospitalized. And yet of the 144 medical schools in the country, there are
only 6 departments of geriatric medicine. Of the nearly 10,000 physicians
who graduated from family practice and internal medicine residency programs,
slightly more than 3% subsequently entered geriatric medicine fellowships. In
2001, there were only 9,000 certified geriatricians.

 Return to Social Gerontology
Index
Return to Social Gerontology
Index
 In our death-denying culture where one dies a series of mini deaths before
physiologically
expiring, where the dying process can be stigmatizing for both the dying and survivors-to-be,
the nursing home industry has emerged as depersonalization machines to absorb the shock of
the dying process. As Richard
Garvin and Robert E. Burger wrote in Where They Go to Die: The Tragedy of America's
Aged (1968), nursing homes are the "halfway houses between society and the
cemetery." In 1996, about $80 billion was spent on the care of 1.6 million Americans--
two-thirds of whom are women--residing in more than 17,000 nursing homes.
Three years earlier, in 1993, it was estimated that the use of nursing homes
would grow by 76% over the next 30 years.
In our death-denying culture where one dies a series of mini deaths before
physiologically
expiring, where the dying process can be stigmatizing for both the dying and survivors-to-be,
the nursing home industry has emerged as depersonalization machines to absorb the shock of
the dying process. As Richard
Garvin and Robert E. Burger wrote in Where They Go to Die: The Tragedy of America's
Aged (1968), nursing homes are the "halfway houses between society and the
cemetery." In 1996, about $80 billion was spent on the care of 1.6 million Americans--
two-thirds of whom are women--residing in more than 17,000 nursing homes.
Three years earlier, in 1993, it was estimated that the use of nursing homes
would grow by 76% over the next 30 years. 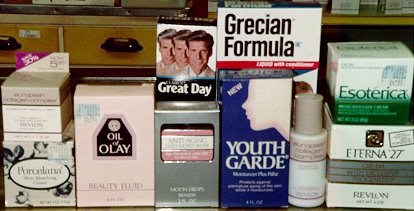

 According
to a report ("Geriatric
Medicine Training and Practice in the U.S. at the Beginning of the 21st Century")
of the American Geriatrics Society, in 1999, though comprising roughly 13% of
the total population, Americans 65 and older made 25% of the office visits to
physicians and were more than twice as likely as the overall population to be
hospitalized. And yet of the 144 medical schools in the country, there are
only 6 departments of geriatric medicine. Of the nearly 10,000 physicians
who graduated from family practice and internal medicine residency programs,
slightly more than 3% subsequently entered geriatric medicine fellowships. In
2001, there were only 9,000 certified geriatricians.
According
to a report ("Geriatric
Medicine Training and Practice in the U.S. at the Beginning of the 21st Century")
of the American Geriatrics Society, in 1999, though comprising roughly 13% of
the total population, Americans 65 and older made 25% of the office visits to
physicians and were more than twice as likely as the overall population to be
hospitalized. And yet of the 144 medical schools in the country, there are
only 6 departments of geriatric medicine. Of the nearly 10,000 physicians
who graduated from family practice and internal medicine residency programs,
slightly more than 3% subsequently entered geriatric medicine fellowships. In
2001, there were only 9,000 certified geriatricians.
